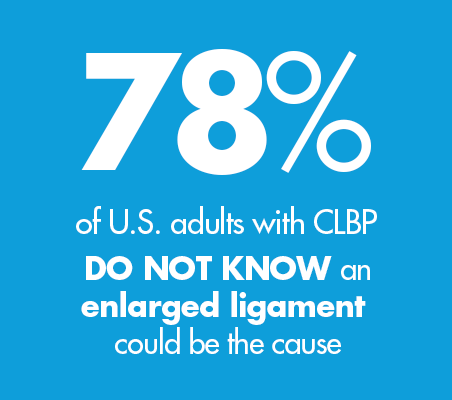
According to Mobility Matters: Landmark Survey on Chronic Low Back Pain (CLBP) in America1:
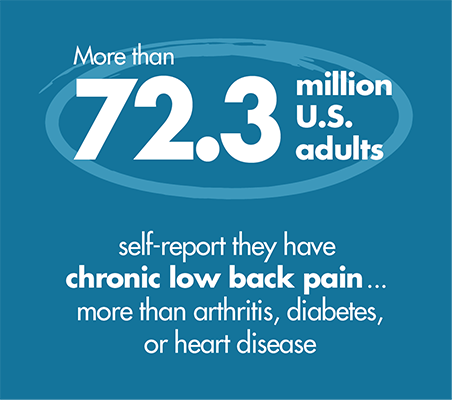
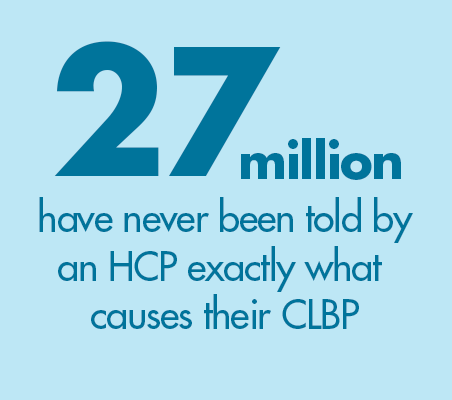
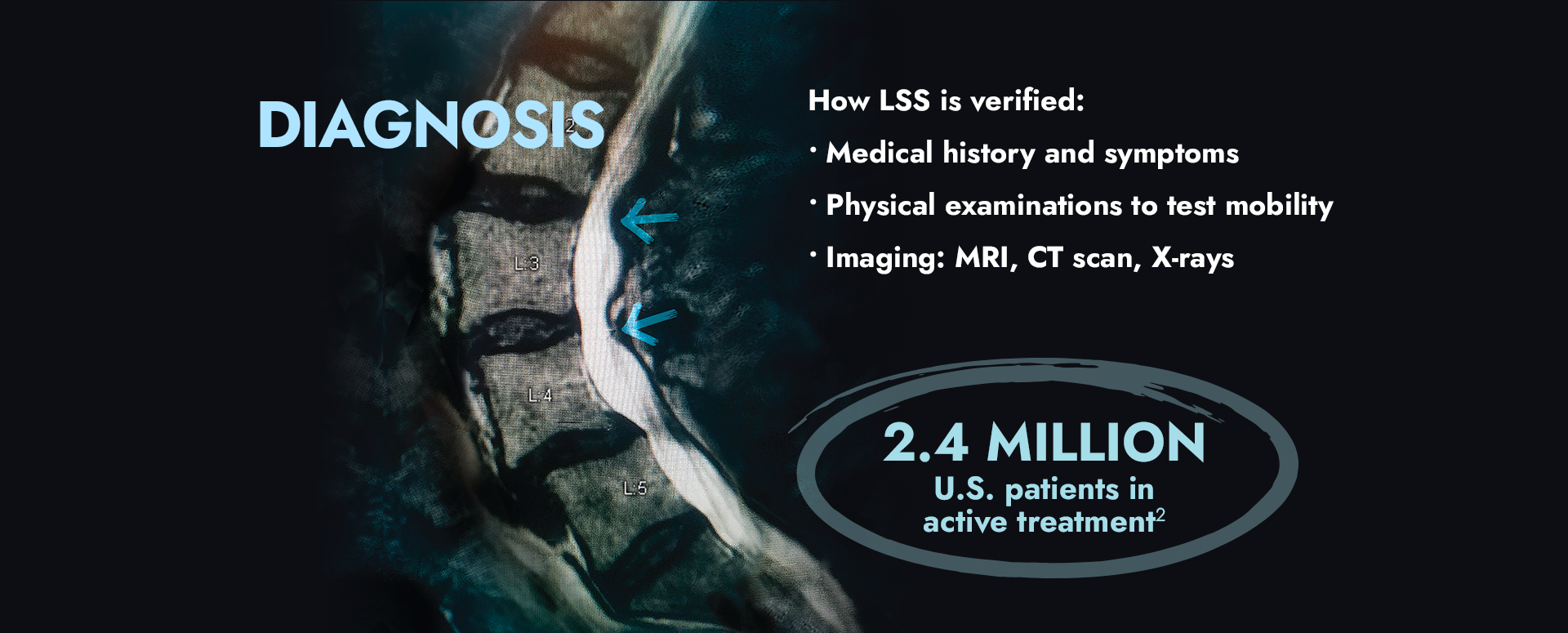
Lumbar spinal stenosis, or LSS, is a common cause of low back and leg pain. In fact, there are 2.4 million U.S. patients in active treatment.2 LSS is generally found in people over the age of 50, and the likelihood of developing LSS increases with age. Learn more about LSS here.
THE MOVING BACK
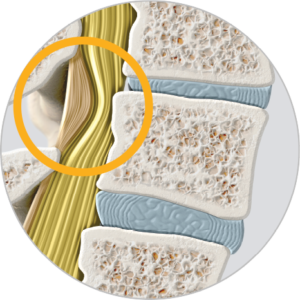
Your back is a marvel of architecture—bone, muscle, and ligament working together to hold you up, move you through life, and protect the spinal canal which sends information to all parts of your body. Understanding that architecture can help you better understand how aging, degeneration, injuries, and other factors can lead to conditions that can cause low back and leg pain, like when an enlarged ligament compresses spinal nerves.
LUMBAR SPINAL STENOSIS & THE ENLARGED LIGAMENT
Lumbar spinal stenosis (LSS) is a condition in which the lower spinal canal narrows and compresses the nerves in the lower back. Up to 85% of spinal canal narrowing is caused by an enlarged ligament.3
Best visualized as a “kink in a drinking straw,” this compression can contribute to pain and mobility issues.
SYMPTOMS
PAIN, NUMBNESS, tingling, or heaviness in the low back, legs, or buttocks when standing/walking.
TEMPORARY RELIEF when bending forward while sitting or standing as pressure on the spinal cord is released and space in the spinal canal is “opened.” Common actions include finding a chair, leaning over shopping cart, using walker or cane.
CAUSES
The natural wear and tear on the spine as people age can lead to a number of contributing factors that cause the narrowing of the spinal canal and create pressure on the spinal nerves:
- Enlarged Ligament
- Bone Overgrowth
- Disc Bulge


LOW BACK PAIN & LSS TREATMENTS
The following chart compares several options that are typically recommended for LSS patients when conservative therapies (eg, physical therapy, pain medication, chiropractic) are not providing adequate relief. Every therapy has risks and benefits. Only you and your doctor can decide which option is best for you.4
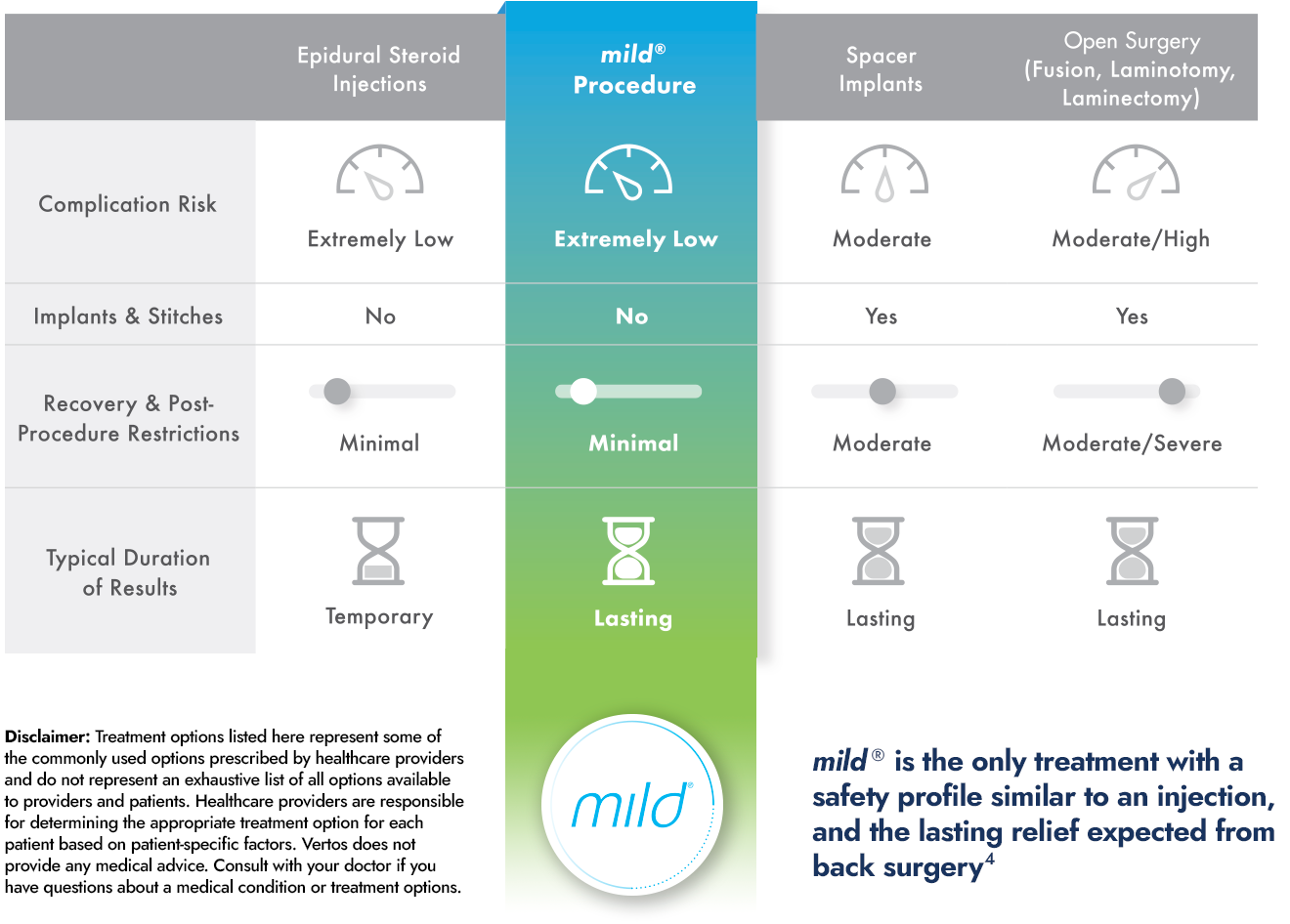
Best Practices for Minimally Invasive Lumbar Spinal Stenosis Treatment 2.0 (MIST): Consensus Guidance from the American Society of Pain and Neuroscience (ASPN)
Published May 5, 2022
ASPN created a guidance for best practice for minimally invasive surgical treatment of symptomatic spinal stenosis. The paper includes explanations, advantages, and limitations of available treatment options.


1Mobility Matters: Low Back Pain in America, Harris Poll Survey, 2022. View data and full summary at knowyourbackstory.com. 2All payor claims analysis. 3Hansson T, Suzuki N, Hebelka H, Gaulitz A. The narrowing of the lumbar spinal canal during loaded MRI: the effects of the disc and ligamentum flavum. Eur Spine J. 2009;18(5):679-686. Doi:10.1007/s00586-009-0919-7. 4Jain S, Deer TR, Sayed D, et al. Minimally invasive lumbar decompression: a review of indications, techniques, efficacy and safety. Pain Manag. 2020;10(5). https://doi.org/10.2217/pmt-
View outcomes, data, full citations, and safety information at www.Vertosmed.com.